Bacterial populations evolve over time to resist antibiotics, and in a growing number of cases around the world, there are infections against which no anti-bacterial medications work at all.
In one particularly worrisome example, certain strains of Enterobacteriaceae (a large bacterial family that includes Escherichia coli and Klebsiella pneumoniae) are resistant to powerful antibiotics called carbapenems. Almost half of hospitalized patients in the United States who get bloodstream infections from these strains will die, according to the Centers for Disease Control and Prevention (CDC). Some other people survive only by getting a decades-old antibiotic with potentially grim side effects.
Novartis scientists now have discovered a compound that aims to attack many of these dangerous bacterial strains. Discovery of this agent, known as LYS228, is being reported at the American Society for Microbiology (ASM) MICROBE meeting in June. The compound is in a first-in-human study to evaluate its safety and pharmacokinetics.
Going Gram-negative
Gram-negative bacteria, including Enterobacteriaceae, protect themselves from the outside world with two very different cell membranes and a variety of efflux pumps. The two cell membranes make an extremely effective barrier that is difficult for many drugs to penetrate. The efflux pumps flush out many of the drugs that are able to penetrate one or both of these membranes.
“You have a hard time getting compounds into bacteria, especially Gram-negative bacteria, plus safety is a high hurdle for new compounds, because of the high doses required to treat these kinds of infections”, says Folkert Reck, a senior chemist at NIBR’s infectious diseases group. These hurdles make new antibacterial discovery very challenging. As a result, no new systemic class of antibiotics against Gram-negative bacteria has been launched in decades.
Existing classes, however, generally work very well against susceptible bacterial strains. Among the most successful are the beta-lactams, which typically kill bacteria by fouling up their cell walls, and only need to cross one of the two bacterial membranes to be effective. Beta-lactams have been safely used to treat infections for over 50 years.
Gram-negative bacteria mainly fight back against the beta-lactams by destroying the antibiotics with damaging enzymes known as beta-lactamases. These enzymes come in two main forms: serine beta-lactamases and metallo beta-lactamases.
Gram-negative carbapenem resistant bacteria in hospitals around the world can be armed with either or both forms of these enzymes. But almost all of today’s beta-lactam drugs, including the carbapenems, can be destroyed by metallo beta-lactamases. It’s a serious problem because carbapenems are often medicines of last resort.
To fight back against these difficult bugs, Novartis researchers decided to develop a new compound from an existing class of beta-lactam antibiotics called monobactams. Monobactams are not able to be destroyed by metallo beta-lactamases, so the team started with the monobactams and invented new compounds that are also difficult to destroy by many of the important serine beta-lactamases.
The US Food and Drug Administration (FDA) approved the first monobactam 31 years ago and LYS228 was built with the tools of modern drug development. One major resource was a library of E. coli strains that were genetically identical except that each came with a different type of beta-lactamase enzyme. By testing compounds against these strains, Novartis scientists determined how each enzyme impacted the ability of the compounds to kill E. coli. “This allowed us to make compounds stable against a variety of different enzymes”, Reck says.
“We also used panels of bacteria from patients to check if we could kill the strains isolated from their infections”, says Jennifer Leeds, executive director of antibacterial discovery at NIBR. “Next-generation sequencing let us look at some of those clinical strains much more closely than we could in the past”.
Decades of learning about beta-lactams helped the Novartis scientists study and optimize compound candidates for efficacy, safety, metabolic stability and interaction with other drugs—including other antibiotics, since these drugs often are combined to confront stubborn infections.
Once LYS228 emerged as the lead compound, Novartis put a major effort into optimizing synthetic routes for the antibiotic. To overcome these synthetic chemistry hurdles, “Novartis chemists around the globe responded very passionately to collaborate with our team in California”, Leeds said.
Continuously seeking cures
That passion reflected the widespread concerns about antibiotic resistance, the Novartis scientists say.
“Modern medicine as we know it would change if we couldn’t treat bacterial infections”, comments Peter Pertel, NIBR’s translational medicine head for infectious diseases. “We couldn’t treat common infections, let alone those associated with immunosuppression or cancer chemotherapy. We couldn’t perform complex surgical procedures or organ transplants”.
“Bacteria have been active in biological warfare for millions of years, fighting each other and coming up with their own defense mechanisms”, Pertel says. “If you look at it that way, bacterial resistance really makes sense. It’s natural selection; you can’t really overcome it. We just try to stay ahead of the game”.
Novartis works both to develop novel antibiotic classes and new members of existing classes, such as LYS228. “This is a progressively more challenging space, and we need to stay in it”, says Leeds. “We need continuous discovery to overcome resistance, which isn’t going away. It’s also important to restrict the use of antibiotics to the patients who need them the most, or we risk losing these very precious drugs".
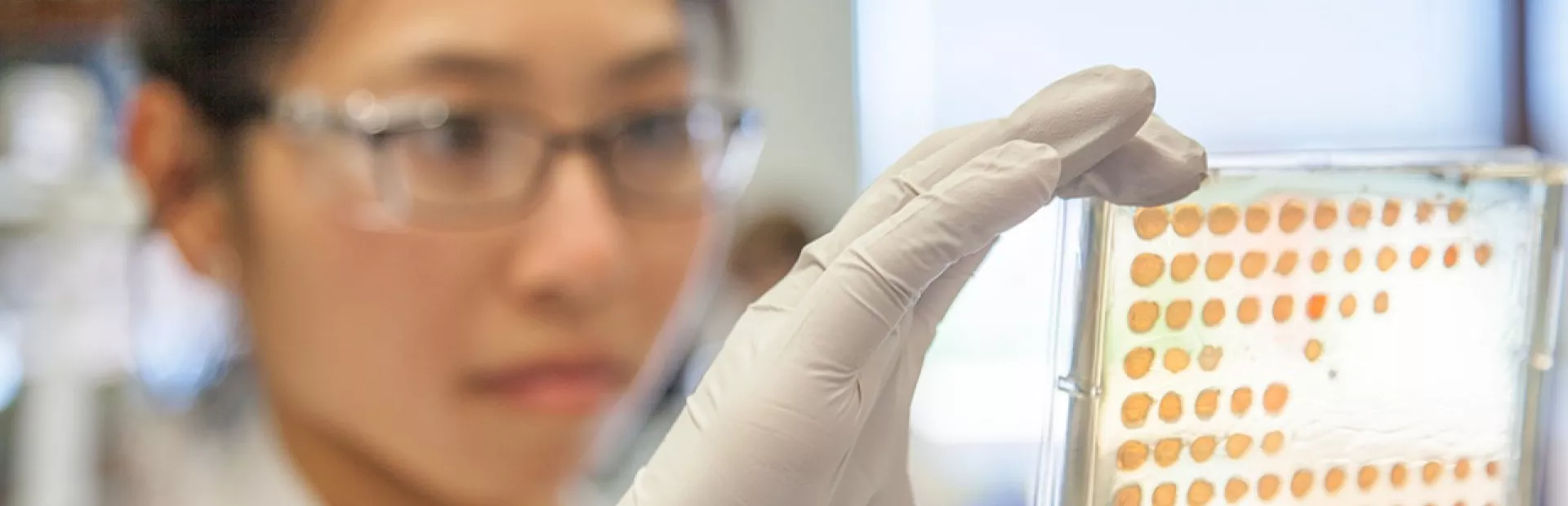
Main image: An Infectious Diseases researcher in Emeryville, California studies the LYS228 compound in the lab.
A new compound aims to attack dangerous antibiotic-resistant bacteria.